In May we celebrate Mental Health Awareness Month, a time where we raise awareness of the toll mental health can have and the many stigmas associated with mental health among many other mental health-related aspects. Through social media campaigns, events and even screenings, organisations across the United States participate in providing key resources for something that affects us all. In that same breath, just as many organisations come together during May to celebrate Asian American and Pacific Islander Heritage Month. The contributions and influence that Asian Americans and Pacific Islanders have made in the U.S. are highlighted and acknowledged. That is why it is only fitting that the intersection between these two is recognised.
While the U.S. categorises many into the term AAPI, we understand and recognise that encompassed within are a wide range of unique and diverse identities, countries, nationalities, and ethnicities. Many who have not only experienced great joy and achievement but unfortunately have also experienced a variety of different challenges, struggles, and trauma. Through the perpetuated model minority myth, various microaggressions, and physical violence, AAPI communities have been and continue to be unjustly treated.
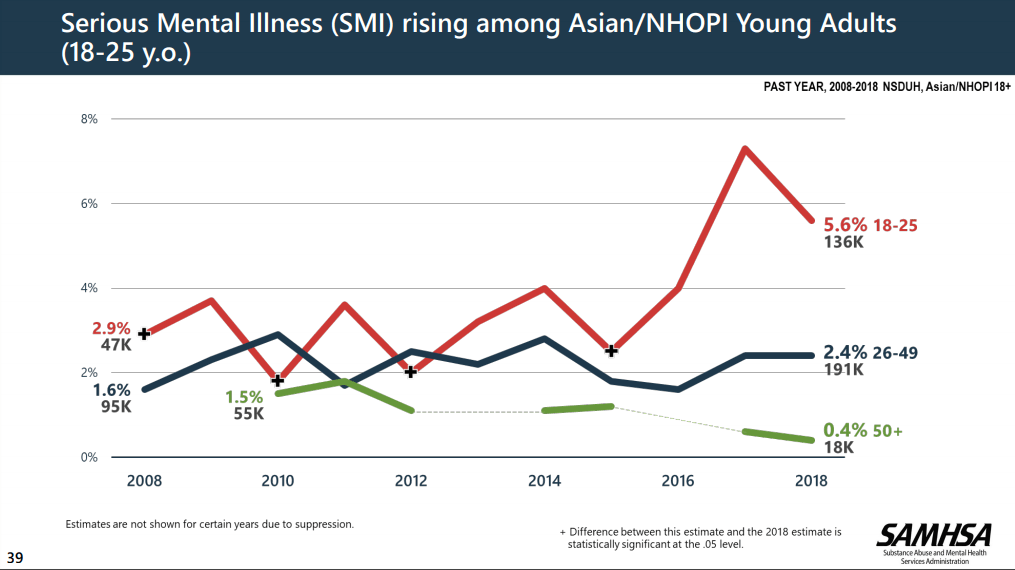
Before we can dive deep into ways to support and resources, understanding barriers to support is the first step as we seek to overcome them. While there are a few, there is still very limited knowledge about AAPI mental health as a result of limited studies which have included individuals from AAPI Communities. “According to SAMHSA’s National Survey on Drug Use and Health, serious mental illness (SMI) rose from 2.9 per cent (47,000) to 5.6 per cent (136,000) in AAPI people ages 18-25 between 2008 and 2018.” (https://www.mhanational.org/issues/asian-americanpacific-islander-communities-and-mental-health)
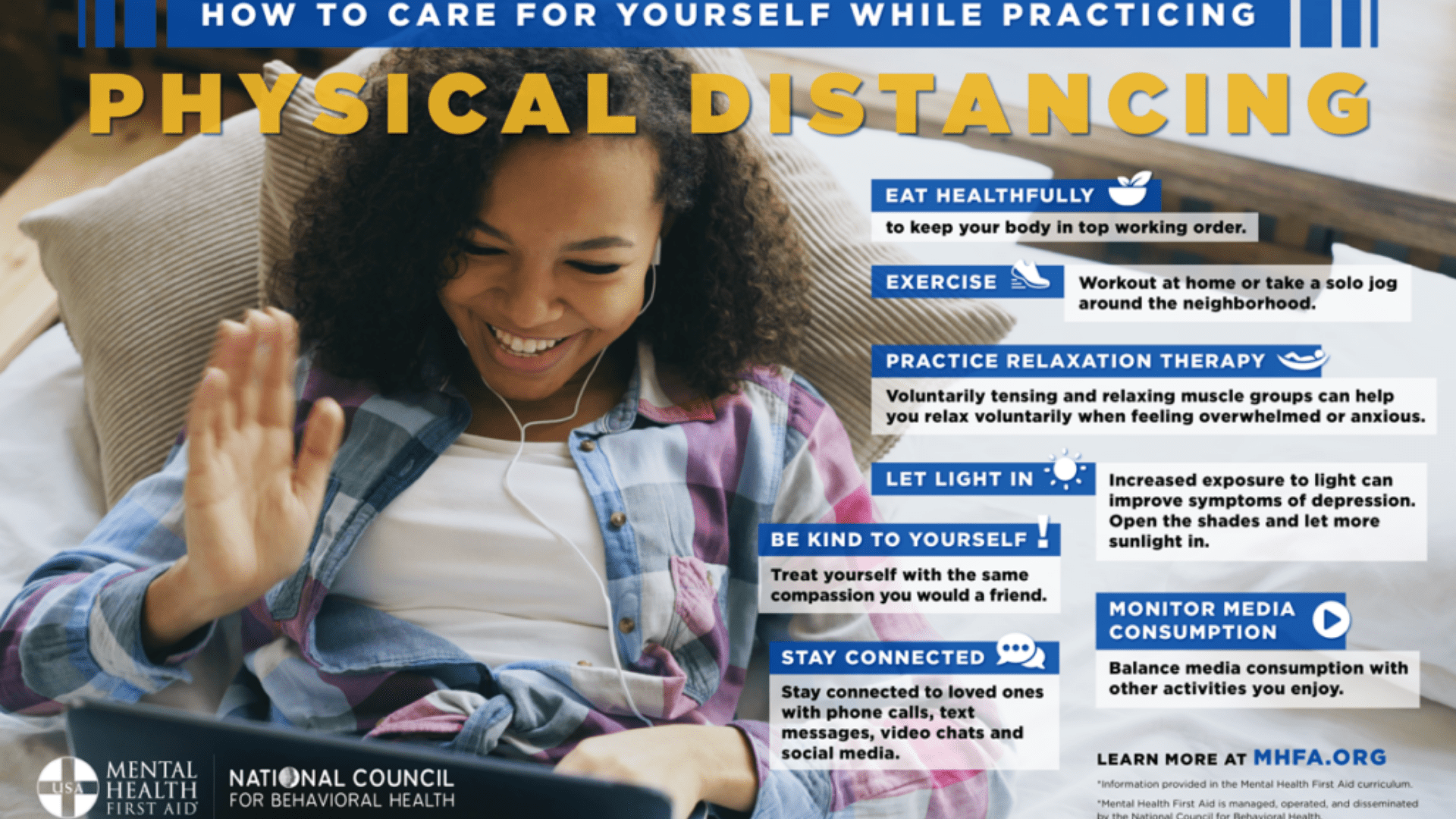
Many young Asian Americans do not seek professional help for their mental concern but rather they turn to their networks. Another thing we see is the lack of awareness for resources along with the still existing stigma around mental health within AAPI communities. This could be considered one of the biggest deterrents for seeking professional help. Other factors include cultural identity, faith, language barriers, and access to insurance and healthcare.
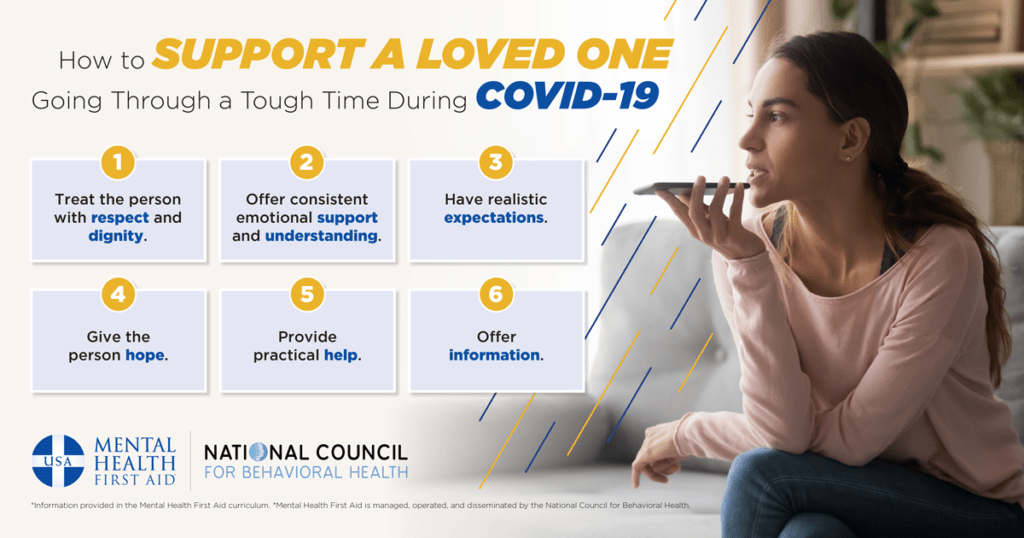
Firstly, as an ally allowing members of the AAPI communities to take charge in spaces and conversations relating to issues they are facing is a major facet of support. Lettings their voices to be the ones heard and amplifying them are good ways to start. Being mindful of language and phrases used when speaking about or addressing members of AAPI communities is also important. Ensuring that stigmatising or stereotypical words are not used and accepting correction can go a long way; again listen to what members of the communities are saying. Additionally don’t be afraid to reach out and show solidarity and support. Check-in and provide resources when you come across them. This goes back to the conversation about de-stigmatisation of mental health issues, show you care with a listening ear (if you have the bandwidth to do so!). Lastly, simply asking, “how can I support you” allow whoever it is to be in charge of the way they receive support. Do they need you to just be that listening ear? Do they just want a space to talk through things and need resources to do so? The answer only comes when you respect their dignity and ask.
For those seeking resources whether for themselves or others, here are some both on and off-campus.
Some resources at DePaul include the APIDA Cultural Center within the Office of Multicultural Student Success, the Office of Health Promotion and Wellness, and University Counselling services.
Off-campus, the Asian & Pacific Islander American Health Forum is focused is improving health among Asian Americans, Native Hawaiians, and Pacific Islanders. The National Asian American Pacific Islander Mental Health Association has a wealth of resources including a directory of mental health service providers for Asian Americans, Native Hawaiians, and Pacific Islanders as does southasiantherapists.org which is a directory of South Asian therapists of various heritages. The University of Connecticut’s Asian and Asian American Studies Institute partnered with the #IAMNOTAVIRUS campaign and the Asian American Literary Review to provide a Mental Health Workbook that includes literature, journals, and lots more resources to support Asian American mental health.