First, the Office of Health Promotion and Wellness wants every Blue Demon to know that all emotions and perspectives concerning the return to campus are valid. Like many other campus organizations, we have warmly (and safely) welcomed the DePaul community back into our office while still providing a number of trainings and resources in virtual settings. This is just one of the ways we are continuing to support DePaul University holistically.
As our community begins the transition back to campus it is likely that we all will experience a mix of emotions. For some of us, it feels exciting to connect with our colleagues on campus again or meet our peers in-person for the first time. Kinesthetic and hands-on learners have the opportunity to engage with class content in a way that better suits their needs. And individuals who lived alone during the pandemic get to reintroduce more face-to-face interactions into their daily routine.
However, for others, returning to campus may be a cause for more stress. Individuals who don’t live close to campus have to once again allocate time for commuting. Those who joined DePaul after March 2020 are learning how to connect with our community in physical spaces. All of us are likely facing anxiety about how to interact with each other in-person while keeping ourselves and our communities safe. It’s even possible to experience feelings at both ends of this spectrum.
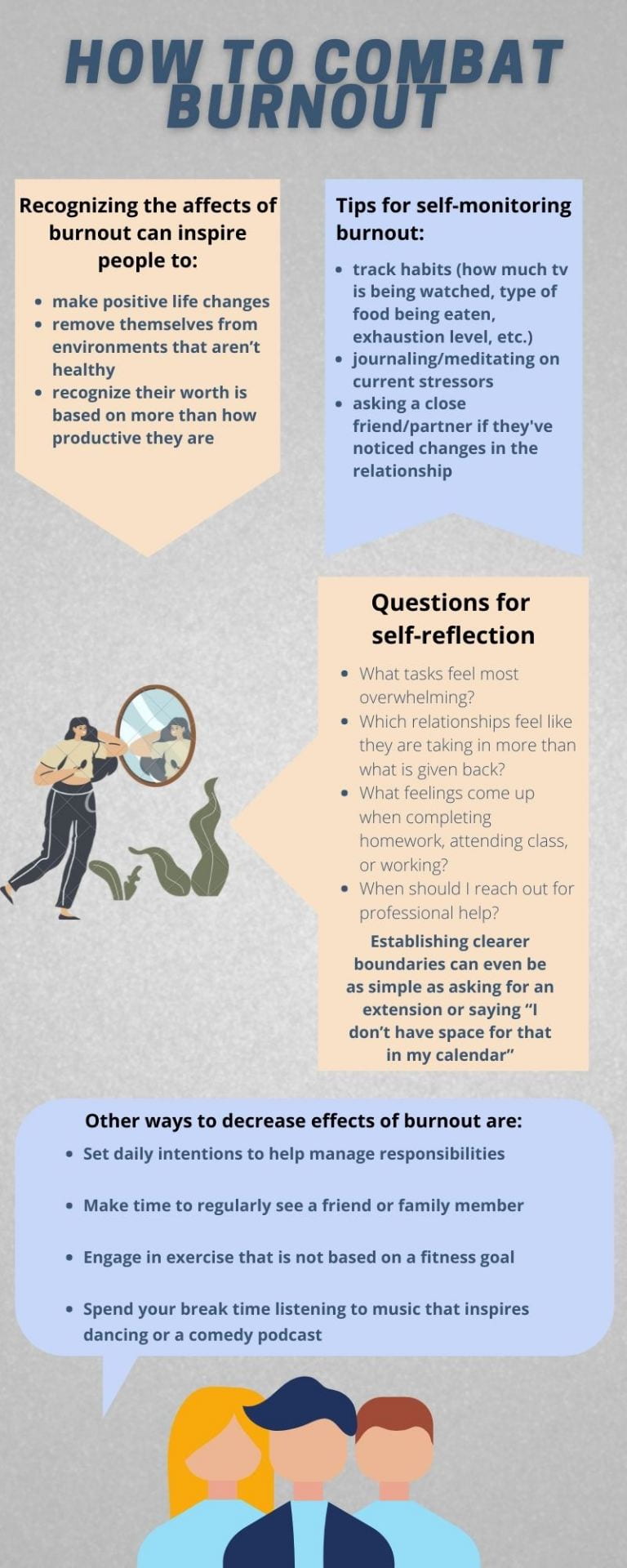
So how do we deal with these complex emotions while maintaining our academic/occupational responsibilities, upholding safety protocols, mitigating social anxiety, and respecting any new boundaries we might have with the return to in-person activities? The first step is giving ourselves time to process what our emotions and needs are. When feeling overwhelmed it is sometimes easy to just focus on how stressed we are or how much we have to do. But it is more important than ever to create space to decompress from our days and practice mindfulness. While meditation is a form of mindfulness that some people do find useful it may not be the best mindfulness tool for everyone. Some other mindfulness techniques can include exercising, journaling, actively listening to music (focusing on the specific words and instruments that evoke strong emotions), cooking a meal, or coloring/crafting. To learn more about how you can incorporate mindfulness into your daily routine read this article by mindful.org: 5 Simple Mindfulness Practices for Daily Life.
Another important habit we can all incorporate into our routines to decrease our stress levels at this time is to regularly reflect on how the return to in-person is affecting our wellbeing. Utilizing reflection to process our experience with returning to in-person can help us understand how our boundaries have changed over the last year and a half. Not only has this time caused us to assess the policies our school and workplaces have concerning sick days/mental health days it has also made many people think about how the organizations we interact with are supporting our needs and engaging in discussions about making their spaces more equitable and accessible. There are internal and external methods of reflection (thinking through the topic, writing pro/con lists, discussing reflections with a loved one, journaling, etc.). Similar to mindfulness, there is no one correct way to engage in reflection. The important part is giving ourselves the time to be honest with how we are being affected so we can be intentional with our boundaries, how we ask for support, and how we interact with our academic, occupational, and personal spaces.

We all deserve to give ourselves and others more grace as we figure out how to acclimate to a new “normal.” By spending more time validating our own feelings we can have more space to validate the feelings of those around us. This is another way we can take care of ourselves, take care of each other, and take care of DePaul.
Resources:
https://www.mindful.org/take-a-mindful-moment-5-simple-practices-for-daily-life/